Salvatore Vendemmia - Aversa, Vito Ferrara - Rome, Ilaria Pezone - Aversa, Domenico Perri - Aversa, Maria Vendemmia - Naples
INTRODUCTION
Hypersensitivity disorders are the expression of exaggerated or not appropriate towards foreign antigens, include allergies, atopies and those that are wrongly directed against components of our body, and that are defined "diseases autoimmune".
CLASSIFICATION
We distinguish four types of hypersensitivity reactions
TYPE I: IgE, immediate hypersensitivity (from a few minutes to almost an hour)
TYPE II: natural stone damage (5-8 hours)
TYPE III: igg, immunocomplex damage (days)
TYPE IV: Damage caused by T cells (delayed hypersensitivity, 48 to 72 hours).
Such different types occur because the immune system reacts towards an antigen. These excessive responses are mediated by antibodies or T cells, and allowed us to identify 4 prototypes of reaction damage immunological. Types I, II, III are mediated by antibodies, type IV is mediated by T cells.
TYPE I, IMMEDIATE HYPERSENSITIVITY (Allergy or Atopy)
This pathology is mediated by IgE. The antigen binds to IgE already bound to tissue mast cells and Basophilic blood granulocytes, and triggers a process of release of additional and harmful mediators. Those preformed represented by histamine, hemotactic and protease factors and synthesized leukotrienes, prostaglandins, cytokines, platelet activators.
These mediators cause vasodilation with increased capillary permeability, hyperproduction of mucus, spasms of smooth muscles and infiltration of eosinophils into tissues, type 2 helper T cells and other cells that aggravate the inflammatory process.
Immediate or type I hypersensitivity is commonly referred to as allergy or atopy, generally manifests after a few minutes, affects about 40% of people and occurs when the subject comes into contact with allergens generally harmless, towards which you are previously sensitized.
We come to contact with dietary and inhalant proteins, and some of these can allergens. Allergens are not only represented by pollen, but also by allergens. Allergens are not only represented by pollen, but also by feces of mites, insect poisons, drugs, etc.
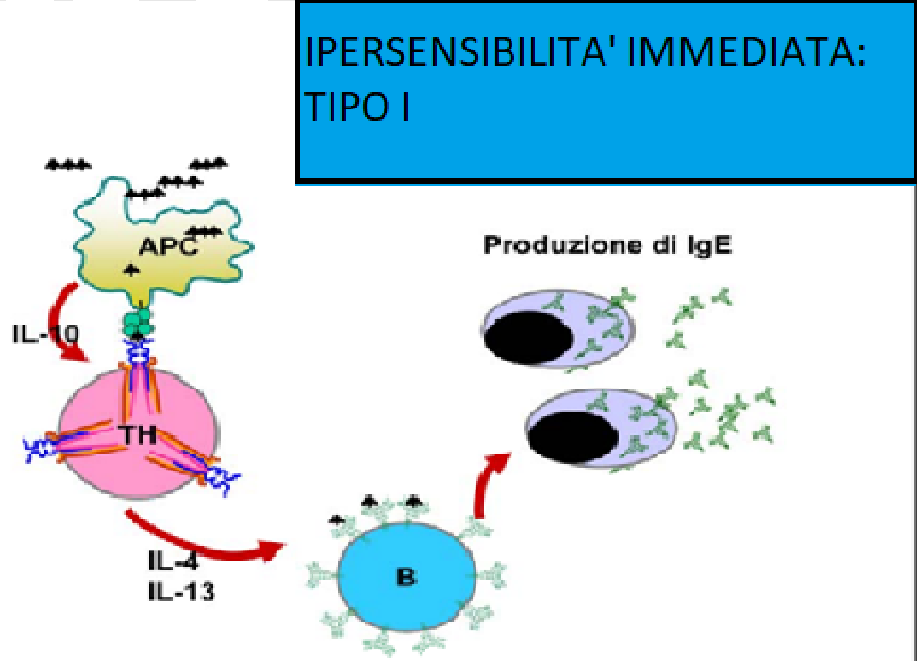
Type I hypersensitivity originates with the activation of specific helper T cells towards the peptides of HLA molecules. Once activated the T helper cells release IL-4 and IL-13, cytokines that activate the B lymphocytes whose BCR binds the allergen, and guide differentiation towards the production of IgE. (Figure 1)
Figure 1
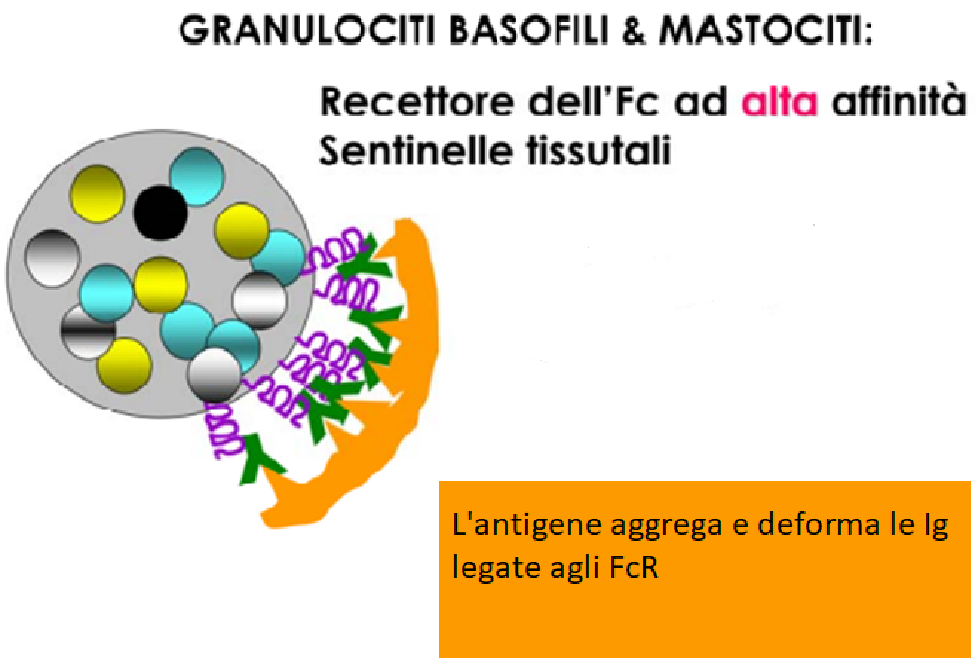
IgE binds to the heavy chain receptor of IgE ; this receptor is present on mast cells and the basophilic granulocytes. The binding of the allergen to IgE anchored to the plasma membrane of mast cells and basophils, leads to deformation of IgE and Fc receptors resulting in cell activation and subsequent degranulation. (Figure 2)
Figure 2
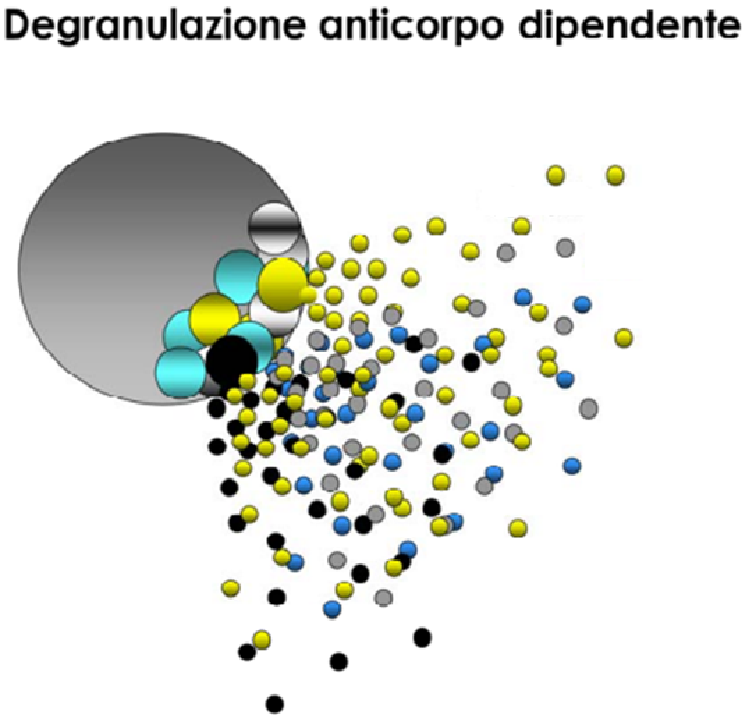
Degranulation of basophils and mast cells causes the release of granules containing histamine, protease, prostaglandins and cytokines (TNF and IL-4) (Figure: 3)
Figure: 3
TYPE I - SYMPTOMS
Clinical manifestation depends on the amount of IgE present in the patient, by the pathway of introduction of antigen and dose.
The most serious and dangerous form of immediate hypersensitivity is SYSTEMIC ANAPHYLAXIS, caused from the massive degranulation of mast cells and basophils in almost all tissues of the patient who presents with dangerous oedemas,especially at the laryngeal level, with sudden fall of the blood pressure. If the allergen is introduced in small quantities, the reaction is milder and bearable: rhinitis, sinusitis, eczema, asthma.
In some individuals a genetic predisposition to allergy has been found: it consists in having HLA molecules that present peptides of an allergen, and have TCR that recognize with ease the HLA-peptide complex.
In other subjects the genetic predisposition is represented by the production of greater amounts of IL-4 and IL-13 which more efficiently stimulate B cells to produce IgE specifications.
Atopic diseases affect the eyes, skin, nose, lungs and are mainly represented by: atopic dermatitis, urticaria, conjunctivitis, angioedema, allergic asthma,rhinitis allergic, reactions to poisonous bites.
We must remember that,generally, ATOPY means an exaggerated IgE mediated immune response. All atopic diseases are Type I hypersensitivity disorders.
For ALLERGY we indicate any excessive immune response to a foreign antigen, regardless of the mechanism.
TYPE II: LYTIC ANTIBODY DAMAGE
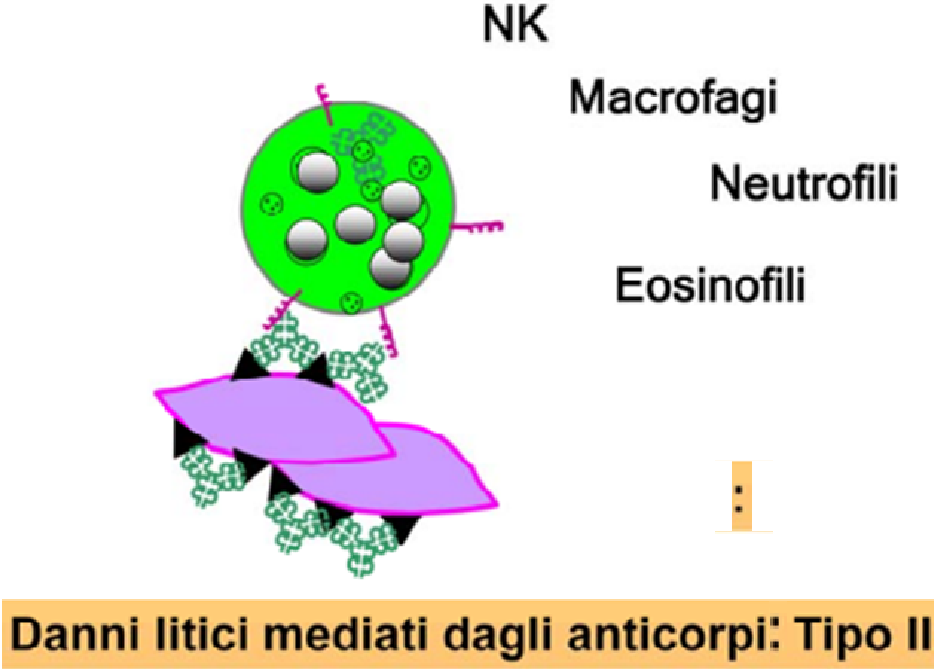
This pathology is caused by antibody-dependent cytotoxic hypersensitivity and occurs when the antibody binds to superficial cell antigens, or to a molecule bound on the cell surface. The antigen-antibody structure that is formed, activates the cells that generate cell-mediated antibody toxicity and/or dependent complement.
Tissue cells are destroyed by NK cells, neutrophils and eosinophils with antibody dependent cytotoxicity mechanism (ADCC) Fig. 4
Figure 4
In different cases, by complement, the binding of antibodies to tissue antigens, determines cell lysis. Leukocyte receptors, activated by the complement cascade, release reactive oxygen radicals and proteollitic enzymes that further damage the affected tissues.
The anaphyltoxins released by the activated complement generate a chemotactic action that increases the number of cells involved in the process. Figure 5
Figure 5
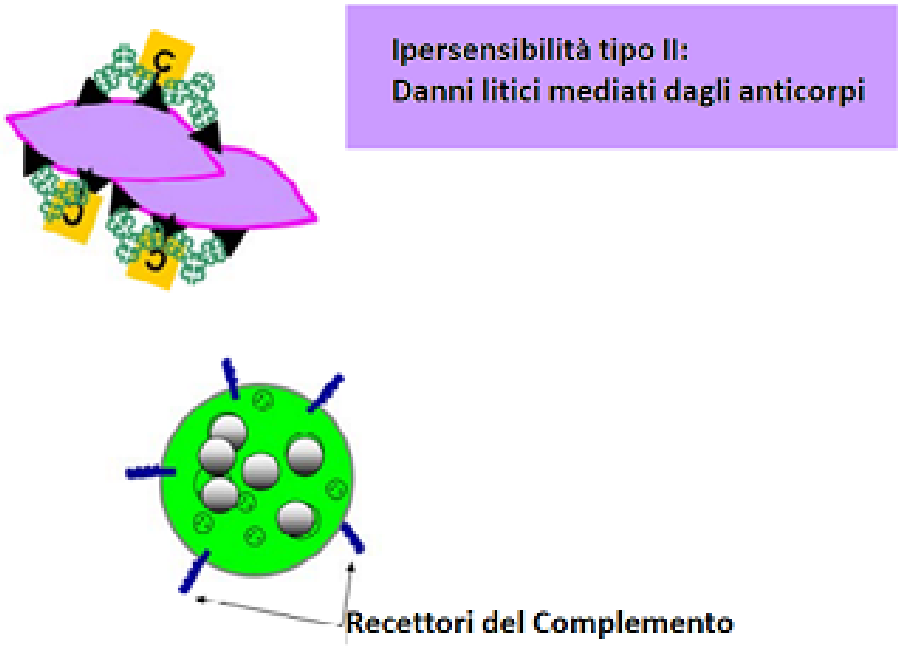
Unfortunately many leukocytes are equipped, in addition to the receptor for the Fc fragment of antibodies, also of the C3b receptor, a protein originating from the complement activation cascade.
Concluding the pathologies mediated by type II reactions include: hyperacute rejection of organ transplantation, hemolytic anemias Coombs positive, Hashimoto thyroiditis, syndrome of Good-Pasture (disease by antibodies to the basal membrane glomerular), and many other.
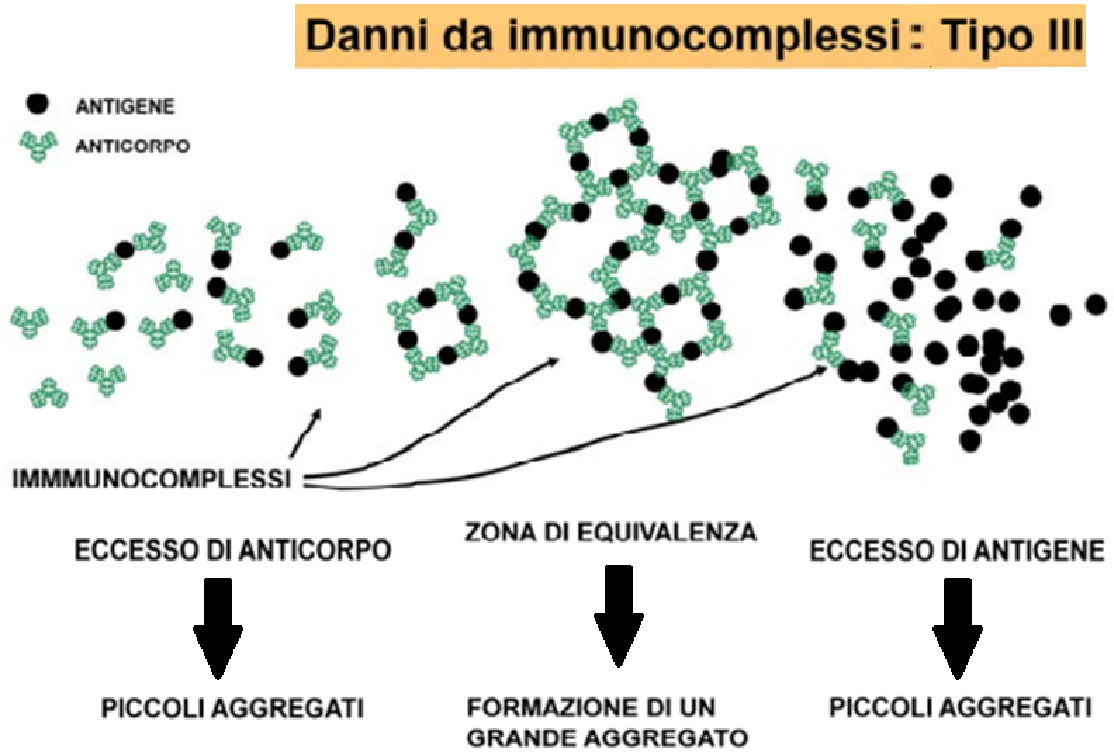
TYPE III --- IMMUNOCOMPLEX DISEASE
This disease is generated by an inflammatory process as a response to deposition, in the vessels and in the tissues, of circulating antigen-antibody immunocomplexes. Such immunocomplexes can activate the complement system or bind to particular immune cells activating them and causing the release of mediators of inflammation. Fig.6
Figure 6
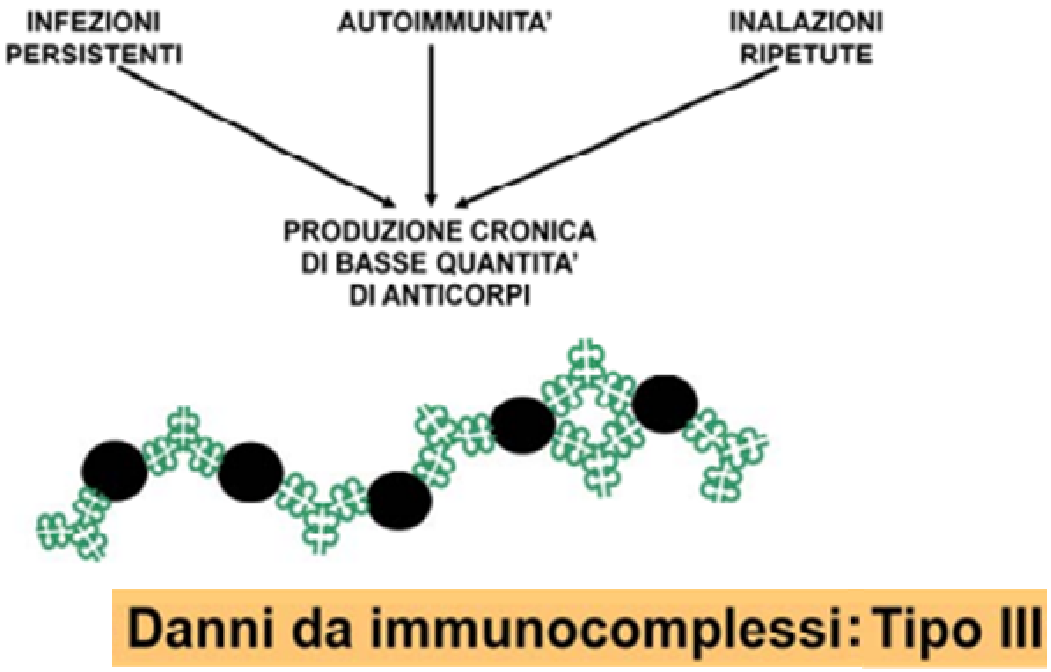
When immunocomplexes are produced in large quantities they can no longer be disposed of from red blood cells and cells with phagocytic activity, which occurs under normal conditions.
Immunocomplexes are formed and dissolved in relation to the amount of antibody and antigen present in the body.
Under normal conditions also a large amount of antibodies generated by the immune response towards a microbial antigen, does not give rise to immunocomplexes (Fig: 7)
Figure 7
Usually small amounts of immunocomplexes are formed which are physiologically eliminated erythrocytes with receptors for complement proteins. Leukocytes can also eliminate them because, in addition to possessing receptors for complement proteins, they possess also the receptor for the Fc fragment of the igg (fig: 8).
Figure 8
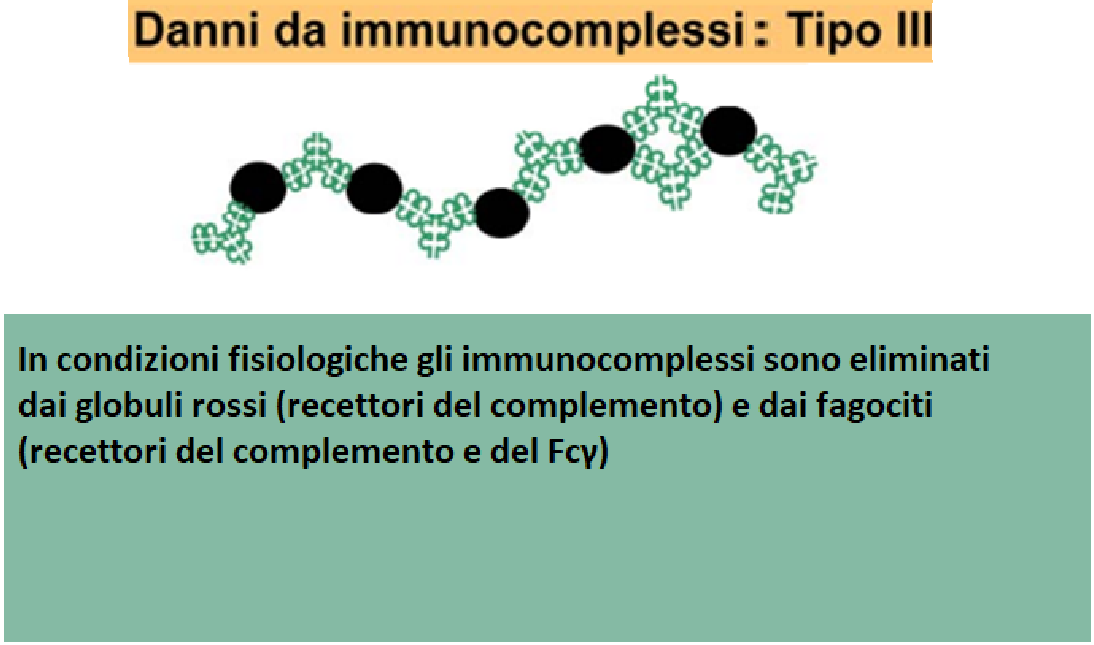
Unfortunately with the introduction of high amounts of antigen or due to the presence of iinfections chronic, large quantities of immunocomplexes are formed continuously that is not possible eliminate.
When the immune complexes settle in the tissues, the complement is activated, they are identified leukocytes expressing the Ig Fc receptor and receptors for factors complementary. This activates a chronic inflammatory process: immunocomplexes accumulate in the blood vessels and renal glomeruli causing chronic diseases: nephritis, arteritis, vasculitis.
HYPERSENSITIVITY REACTIONS TYPE IV
They occur 2/3 days after the introduction of the antigen that causes the reaction. The delay is due because this pathology is mediated by T cells and not by antibodies.
These delayed reactions manifest themselves towards numerous antigens that activate TCD4+ lymphocytes and CD8+, and cause obvious lymphocytic infiltration and edema in the area where it has infiltrated the triggering antigen.
Activated CD4+ lymphocytes allow the release of cytokines that activate a phlogistic process local, and also activate macrophages with which they cause tissue damage.
This damage becomes more pronounced if CD8+ cells are activated. Type IV reactions are: Stevens Johnson syndrome, hypersensitivity pneumonia, necrolysis epidermal blisters, contact dermatitis, etc. in the liver, following viral infections, activation of T cells leads to destruction of infected liver cells resulting in liver tissue damage. This disease is also responsible for the rejection in transplanted, the elimination of aged cells, of those mutated and cancer.
BIBLIOGRAPHY
- Gian Luigi Marseglia, Nuove Prospettive Terapeutiche Nelle Malattie Allergiche. Aggiornamenti in Neonat. e Ped: pagg.135-138 Cuzzolin Editore Napoli Anno 2024
- Pasquale Comberiati Anaphylaxis in children Agg. in Neonat, e Pediatria.pagg.91-93 Cuzzolin Ed. Napoli Anno 2024
- Tejedor Alonso et al. Epidemiology of Anaphylaxis Clin Esp. Allergy 2015 Jun,45(6)11111027-39
- S. Roberts G. et al. Guidelines on effective transition of adolescents and young adults with asthma and allergy - Allergy 2020 Nov. 75(11),2734-2752
- Università degli studi di Torino: https://medtriennalisl.campusnet.unito.it
